Thursday, 29 April 2021
Often, the skin can be a window to what is occurring inside your body. For women with polycystic ovarian syndrome, or PCOS, this this may mean acne, hair loss, excessive facial or body hair growth, dark patches on the skin, or any combination of these issues.
What is PCOS?
Skin and hair issues can be the most readily perceptible features of PCOS, and thus sometimes the reason for seeking medical care. However, features of PCOS also include menstrual irregularities, polycystic ovaries (when the ovaries develop multiple small follicles and do not regularly release eggs), obesity, and insulin resistance (when cells do not respond well to insulin).
The cause of PCOS is not entirely understood, but scientific evidence points to hormonal imbalances, specifically excess testosterone (also known as hyperandrogenism) and insulin resistance. PCOS is the most common cause of infertility in women. The hormonal imbalances in PCOS disrupt the process of ovulation, and without ovulation pregnancy is not possible. PCOS exists on a spectrum, meaning not every woman with PCOS has the same signs and symptoms. Because of the variation in characteristics of this syndrome, it can be difficult to diagnose.
How do I know if I have PCOS?
There is no one specific test that can be used to diagnose PCOS, so a thoughtful and thorough workup, including lab tests and imaging, is needed. Lab tests typically involve measuring levels of various hormones, such as androgens. Imaging tests may include ultrasound of the ovaries. Seeking care from an experienced team, including primary care physicians, gynecologists, endocrinologists, and dermatologists, can establish the diagnosis.
What are the skin manifestations of PCOS?
PCOS-related acne often flares on the lower face, including the jawline, chin, and upper neck. Although not a hard and fast rule, these areas are considered to be a hormonal pattern for acne. Women with PCOS may notice that acne lesions are deeper, larger, and slower to resolve. Acne in PCOS usually worsens around the time of menstrual periods. Dermatologists often recommend the use of oral contraceptive pills or a medication called spironolactone to treat this type of acne. These treatments, when used in the right patients who have no contraindications to them, can be very helpful in clearing acne.
Hirsutism, or excessive hair growth in places where hair is usually absent or minimal, is another dermatologic sign of PCOS. Common areas of hirsutism include the chin, neck, abdomen, chest, or back. On the scalp, however, balding or thinning of the hair can be seen. Both of these hair issues are driven by an excess of testosterone.
Occasionally, another skin condition appears called acanthosis nigricans, which are dark, velvety areas of skin, usually in skin creases such as around the neck and underarms. This type of skin condition is also associated with insulin resistance, and may be due to stimulation of skin cells by insulin, causing them to overgrow.
Treatment options and a tailored approach
Although there is no cure for PCOS, there are many treatment options for managing various symptoms of this syndrome. The types of treatments used depend on a woman’s priorities and symptoms. For example, being at a healthy weight can lead to improvement of symptoms, so lifestyle modifications to nutrition and exercise may help. Hirsutism can be treated with laser hair removal or electrolysis. Some patients may try birth control pills to improve menstrual regularity. Metformin, a commonly used medication for diabetes, can be used to help improve the body’s response to insulin.
Treatment planning is tailored to each person and depends on whether or not pregnancy is a short-term goal. Certain medications, including spironolactone and retinoids for acne, should be avoided if a woman is trying to become pregnant.
The post Polycystic ovarian syndrome and the skin appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/polycystic-ovarian-syndrome-and-the-skin-2021042922502
via IFTTT
Polycystic ovarian syndrome and the skin
Wednesday, 28 April 2021
Keeping your partner — or yourself — up at night with loud snoring? This might be more than a nuisance. About 25% of men and nearly 10% of women have obstructive sleep apnea (OSA), a serious sleep disorder characterized by explosive snores, grunts, and gasps. Tissue at the back of the throat temporarily obstructs the airway, leading to breathing pauses (apneas) throughout the night. Not only does OSA leave people tired and groggy, but it also puts them at risk for a host of health problems, including high blood pressure, depression, and heart disease.
The most effective and best-studied treatment is positive airway pressure (PAP), a small bedside machine that blows air through a mask to prevent your airway from collapsing. But people with mild or moderate OSA sometimes find PAP challenging to use, and often wonder about alternatives. Dental devices (also known as oral appliances) are an option for some people. But do your homework before going this route, cautions Sogol Javaheri, MD, MPH, MA, a sleep specialist at Harvard-affiliated Brigham and Women’s Hospital.
Who might benefit from a dental device for sleep apnea?
“These devices are supposed to reposition your jaw or tongue to open your upper airway. But they can be really uncomfortable and only work about half the time,” Dr. Javaheri says. It’s hard to predict who might benefit from using an oral device, and people with very mild OSA and few symptoms may not notice any difference. As a result, she generally doesn’t recommend them except for people with mild to moderate OSA or those with severe OSA who can’t tolerate PAP.
Three main categories of dental devices for OSA
Mandibular advancement devices. Made of molded hard plastic, these devices snap over your lower and upper teeth, and also feature metal hinges and screws that can be tightened to push your lower jaw forward. Some dentists make custom mandibular advancement devices, but before you consider buying a custom device, be sure to ask whether your dentist has experience in sleep-related breathing disorders and is certified by the American Academy of Sleep Medicine. Some non-certified dentists simply take a mold of your teeth, send it to a company that makes the device, then sell it to you at a large markup — sometimes totaling $4,000 or more. What’s more, it’s unlikely to be covered by your dental or medical insurance if it’s used for snoring.
Mouth guards. Similar to mandibular advancement devices, these devices also help reposition your lower jaw, although to a lesser degree. Some sleep physicians recommend SnoreRx, which you can purchase online for less than $100. Instead of starting with an impression of your teeth created by a dentist, you use what the company calls the “boil and bite” method. You place the device in a cup of boiling water for a minute and then bite down on the softened plastic so it molds to your teeth.
Tongue-retaining devices. These devices consist of a soft plastic splint placed around your tongue that holds it forward and out of your mouth throughout the night. They tend to make your mouth very dry and can be quite uncomfortable.
Most insurance plans at least partially cover these devices when used for OSA, but not if they’re used for simple snoring. Don’t be tempted to try one unless you’ve been formally diagnosed with OSA, says Dr. Javaheri. And even if you have OSA, be sure to call your insurance company so you understand how much is covered before you have a device made.
The post Dental appliances for sleep apnea: Do they work? appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/dental-appliances-for-sleep-apnea-do-they-work-2021042822476
via IFTTT
Dental appliances for sleep apnea: Do they work?
Tuesday, 27 April 2021
No one likes getting stuck by a needle. Whether for a blood test, vaccination, or blood donation, needle sticks are something most people would prefer to avoid.
Yet, judging only by schedules for routine vaccinations and tests, the average healthy person can expect at least 165 needle sticks over a lifetime. Get hospitalized? That might add dozens or even hundreds more. And the number of needle sticks experienced by people with diabetes, HIV, and some other illnesses hovers in the “don’t ask” range.
For many, this may be more of an annoyance than a real problem. But if you have a strong fear of needles or aversion to the sight of blood, getting a vaccination or any other needle stick is a big deal. If this sounds like you, you may have trypanophobia.
What is trypanophobia?
Fittingly, the name combines the Greek term trypano — meaning puncturing or piercing — with phobia, meaning fear. This remarkably common condition is marked by irrational, extreme fear or aversion to blood or needles. It’s estimated that fear of needles affects up to 25% of adults, and may lead 16% of people in the US to skip vaccinations. Many people who strongly fear needle sticks may avoid doctors and medical care, so it’s likely that the magnitude of this problem is underestimated.
Just to be clear: this phobia is not limited to people who are overly sensitive to pain or aren’t “tough enough.” It can affect anyone. The cause is often unknown, but a particularly traumatic experience during childhood medical illness may set the stage for some people. And there may be a genetic component. Researchers have found genes linked to fainting after needle sticks, and trypanophobia sometimes runs in families.
What are the symptoms of this phobia?
People with trypanophobia who are contemplating a needle stick may experience
- fear or anxiety
- panic attacks, nausea, or sweats
- palpitations
- fainting (due to a reflex in which pain or the sight of blood triggers a drop in blood pressure)
- insomnia in the days or weeks before an expected needle stick.
How does being afraid of needles affect you?
This fear can affect your
- quality of life: It’s quite unpleasant to spend weeks dreading an upcoming doctor’s appointment.
- health: Skipping recommended tests and treatment to avoid needle sticks can lead to missed diagnoses, poorly monitored medical conditions, and undertreatment. A timely example is foregoing a vaccination against COVID-19, which can have serious or even deadly consequences. Also, drug marketers sometimes play on fear of needles in their advertising, or might downplay the fact that a medication requires an injection.
- longevity: Skipping routine medical care can contribute to avoidable suffering and death. For example, a cancerous breast lump that might have been detected during routine examination may go unnoticed until much later, when it’s no longer curable.
What can you do to cope with a fear of needles?
There’s not much high-quality research regarding how best to treat trypanophobia. Still, experts suggest a number of options to help people cope with it.
- Bring support, if allowed. That’s routine for small children. But holding the hand or hearing the voice of a spouse, trusted friend, or family member can calm adults, too.
- Harness the power of distraction (see this amazing video of a pediatrician distracting a young child before a vaccination). Focus on anything other than the needle stick: a spot on the floor, the positive effects of getting a COVID-19 vaccine (soon you can hug your family!), or your upcoming vacation.
- Tell the person giving you a shot or drawing blood that you struggle with this, and let them know what works best for you. Some people prefer to hear about each step before it happens so there are no surprises. Ask if the healthcare provider has tricks of the trade to help you get through it.
- Ask the person giving you’re a shot or drawing blood if they can use a numbing agent similar to novocaine, or a freezing spray to numb skin before a needle stick.
- Don’t watch! It’s not helpful to watch all of the preparation for the needle stick or see the needle itself. Watching may make things worse.
- Learn ways to relax. Try deep breathing or other relaxation techniques that you can practice before having the needle stick.
- Relax the muscle receiving the injection, too. Some shots, such as vaccines that protect you against tetanus or COVID-19, are given in a muscle. Relaxing the muscle can lessen the pain of these shots.
- Lie down before having the needle stick, if you’ve fainted or felt woozy in the past with needle sticks.
Can therapy help?
Seeing a mental health specialist may be helpful. He or she may recommend
- cognitive behavioral therapy, or CBT, which teaches people ways to reframe unhelpful ways of thinking and build coping strategies.
- exposure therapy, a gradual and supervised increase in your exposure to needles, which can lessen the panic they cause. For example, over a number of weeks you may be instructed to look at photographs of needles, then hold a syringe without a needle, then hold a syringe with a needle, and then imagine injection — all with guidance from a therapist — before actually having one.
- medications, such as anti-anxiety or sedative medications, may be prescribed if other measures aren’t effective, and the anxiety around needle sticks is getting in the way of medical care (or just making you miserable).
The bottom line
It’s natural to have an aversion to pain, even when you know it’s coming and even though it’s for a good reason. So, if you’re one of the millions fretting about getting a COVID-19 vaccine or a blood test or any other needle stick, know that you’re not alone, and that there are things you can do to improve the situation. Talk to your doctor about your fear and get help if you need it. Your quality of life, health, and longevity could depend on it.
As for me, I’m going to do what I always do: avert my eyes and stare at that spot on the floor.
Follow me on Twitter @RobShmerling
The post Terrified of needles? That can affect your health appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/terrified-of-needles-that-can-affect-your-health-2021042722470
via IFTTT
Terrified of needles? That can affect your health

Indonesian-style vegetarian stir fry with color, crunch, and a kick. Make it a dinner for two for 20g of protein per serving.
The post Green Beans and Tofu With Peanuts appeared first on MyFitnessPal Blog.
from MyFitnessPal Blog https://blog.myfitnesspal.com/watch/green-beans-and-tofu-with-peanuts/
via IFTTT
Green Beans and Tofu With Peanuts
Monday, 26 April 2021
Not long ago, during pre-pandemic 2019, the reported life expectancy at birth for non-Hispanic Black, non-Hispanic White, and Hispanic populations was approximately 75, 79, and 82 years, respectively. The higher life expectancy of Hispanic people compared to others in the United States may come as a surprise to some.
This phenomenon, known as the “Hispanic paradox,” was first noted in the 1980s, and its legitimacy has been debated since. A host of explanations have been proposed, including hypotheses about the “healthy immigrant” (people who migrate to the US are healthier than those who stay in their native countries) and “salmon bias” (less healthy US immigrants are more likely to return to their countries of origin). Other experts note that Hispanic communities have lower rates of smoking and greater levels of social cohesion, which certainly may contribute to their presumed higher life expectancy. In the end, this difference remains poorly understood, and is further complicated by research noting US-born Hispanic individuals may have lower life expectancy compared to their foreign-born counterparts.
Now, recent estimates for life expectancy from the Centers for Disease Control and Prevention (CDC) show an alarming change that highlights the disproportionate impact COVID-19 has had on communities of color. Between 2019 and 2020, life expectancy dropped more sharply among Black and Hispanic populations compared to their White counterparts, by three years, two years, and one year, respectively. In fact, the gap in life expectancy between Black and White populations widened from four to six years, the largest gap since 1998. And the advantage in life expectancy previously held by Hispanic populations over Whites decreased from three to two years. In other words, the COVID-19 pandemic has led to a decrease in life expectancy among all individuals in the US, but this impact has been felt most by communities of color.
Many reasons for greater vulnerability to COVID-19
Many factors contributed to this uneven drop in life expectancy. But these remarkable numbers remind us of the vulnerability of Black, Indigenous, and People of Color (BIPOC) in the US, the result of longstanding unequal access to health care and resources needed to achieve upward economic mobility. Many BIPOC populations in the US live on the brink of collapse. With little health or financial reserves, these communities are increasingly vulnerable to sudden events, like the financial collapse of the early 2000s or a global pandemic.
Racism functions largely through structural barriers that advantage some groups and disadvantage others. Rather than causing new disparities, the COVID-19 pandemic simply unmasked chronic failings in our social policies and healthcare delivery for our BIPOC communities. Recently, the CDC acknowledged this and declared racism a public health threat that harms the health and well-being of BIPOC populations.
Longstanding systemic failings lead to poor overall health
Abnormally high and sustained exposure to stress during pregnancy and early childhood leads to sustained release of inflammatory and stress-related hormones such as cortisol, which results in toxic levels of chronic stress. Racism causes chronic stress, which detrimentally affects the development and well-being of BIPOC children. Moreover, many BIPOC children have less overall opportunity to thrive. They live in neighborhoods plagued by pervasive poverty caused by longstanding discriminatory policies such as redlining and residential segregation. These factors compound, ultimately resulting in higher levels of cardiovascular disease, mental illness, and health-risk behaviors. Known as weathering, this contributes to both decreased lifespan and healthspan (the period of a life during which a person is in good health).
Further, BIPOC individuals in the US persistently face barriers in access to quality health care. Examples include higher rates of no insurance and underinsurance, and lower health care literacy. Pervasive bias and discriminatory policies are deeply embedded into our healthcare delivery infrastructure. So, the results of the CDC report should come as no surprise: a population chronically deprived of accessible preventive services would be expected to fare poorly during a pandemic.
Moving forward: What changes could help?
We can all raise our voices to persuade and support the efforts of government officials at every level, and healthcare leaders, to address immediate disparities related to the ongoing pandemic and the chronic flaws that leave BIPOC communities increasingly vulnerable. Below are several measures that could get our system moving in the right direction.
Regular citizens can
- Vote in all elections — especially local elections. Local elected officials, such as a city mayor, town manager, city council members, and county sheriff, can affect the lives of citizens even more personally than state or federal officials. Local news media and websites may have information on policy views and track records to help you choose candidates.
- Be wary of fake news promoted on social media. Social media places a wealth of information at our fingertips, yet also offers ways to spread false information that can greatly affect our decisions. Try to maintain a healthy level of skepticism. Check information with trusted sources. These common-sense tips can help keep you from falling victim to fake news.
- Support local organizations. Local nonprofits and community organizations play a major role in helping to address COVID-19 disparities affecting BIPOC communities and fighting for testing and vaccine equity. If you’re financially able, consider donating to local nonprofits, food banks, and community organizations so that they can keep helping in times of need.
Policy makers and government leaders can
- Fix unemployment insurance. Inject federal funds into refurbishing crumbling state unemployment insurance infrastructures, and pass legislation mandating that standard minimum benefits be provided by all states.
- Make universal healthcare happen. Ensure universal health insurance is achieved, whether via a public option, single payer, or a host of other alternatives. Americans deserve equitable access to quality healthcare, especially preventive care.
- Eliminate historically racist and discriminatory policies. Eliminate discriminatory practices like gerrymandering that contribute to ongoing disempowerment of voters, residential segregation, and pervasive poverty, leaving communities of color in destitute circumstances without a voice.
Editor’s note: At the request of Dr. Perez, terms used to describe all races and/or ethnicities are capitalized in this post, to reflect his view of identity and racial equity.
The post Life expectancy: How can we address uneven declines? appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/life-expectancy-how-can-we-address-uneven-declines-2021042622466
via IFTTT
Life expectancy: How can we address uneven declines?
Friday, 23 April 2021
If a 3-year-old finds a cookie on the table, chances are they are going to eat it.
Even if it is made with marijuana or THC, CBD, or other components of cannabis.
As more states have legalized the use of marijuana and an ever-widening range of derivative products, it’s not surprising that more children are being exposed — including by eating marijuana edibles. A research brief published in the journal Pediatrics found that between 2017 and 2019, there were 4,172 calls to regional poison control centers about exposures to cannabis in babies and children through age 9. About half of the calls were related to edibles.
The frequency of these calls, and the percentage related to edibles, went up over the two-year period. Not surprisingly, the exposures were about twice as common in states where marijuana use is legal as in those where it is not.
More calls about edibles involving younger children
The most common age group involved was 3- to 5-year-olds, which makes sense: this is the age where they are old enough for parents to take their eyes off them for a minute or two, but not old enough to understand why they shouldn’t eat that brownie, gummy bear, or piece of chocolate.
Thankfully, the effects of these exposures were mostly minor — but in 15% they were moderate, and in 1.4% they were severe. In rare cases, significant ingestion can lead to trouble breathing or even coma. That’s the problem with edibles: it’s hard to know how much cannabis is in each one, it’s easy to ingest a lot, and the effects can last a long time.
It’s important to remember, too, that this was just a study of calls to poison centers. It’s impossible to know how many exposures there have been that were never reported — including how many went completely unnoticed by parents or caregivers.
Safety first: Children and cannabis
Clearly, there will need to be some regulation around labeling and child-safe packaging. But as an immediate step, parents and others shouldn’t buy marijuana edibles that might appeal to children (just like it’s best not to buy detergent pods that look like candy). If you do buy marijuana edibles that a child might want to eat, they need to be stored securely, out of reach, always.
When parents bring their children to visit friends, it may be a good idea to add marijuana edibles to the list of safety issues to ask about. Think of something along the lines of, “Hey, our daughter is still little and curious, so we like to ask about things like matches, guns, medications, marijuana edibles, or other things that might be dangerous for her if she gets into them. Is there anything that might be in her reach?”
It might be a bit awkward, but if you make it quick and routine, you can decrease the awkwardness. And ultimately, it’s worth a bit of awkwardness to keep your child safe.
Follow me on Twitter @drClaire
The post Edibles and children: Poison center calls rise appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/edibles-and-children-poison-center-calls-rise-2021042322450
via IFTTT
Edibles and children: Poison center calls rise
Thursday, 22 April 2021
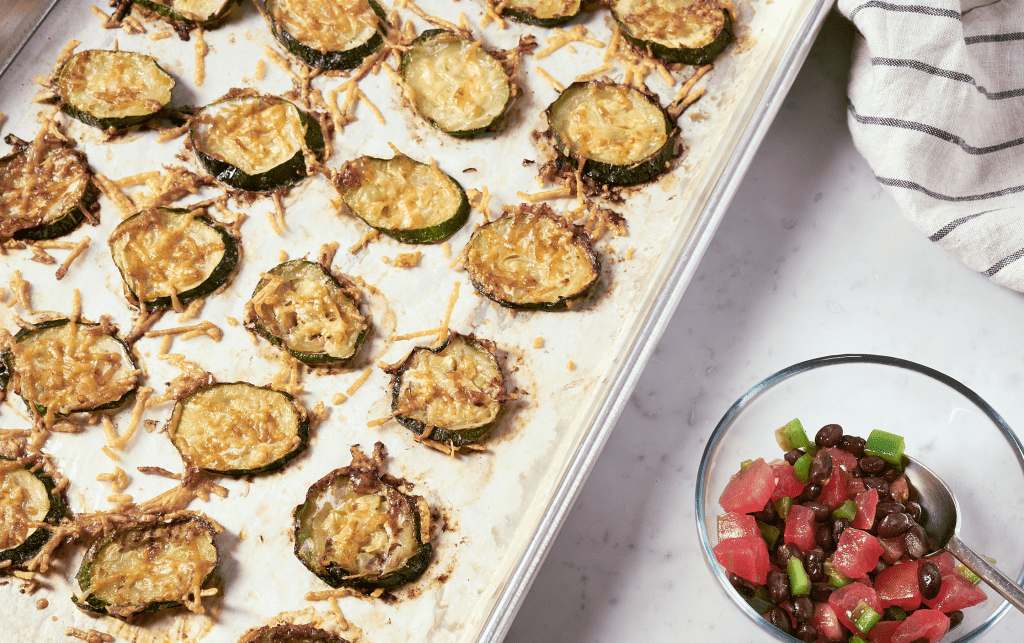
Skip the chips! Crispy sliced & baked zucchini with parmesan is a healthier dipper, and perfect for a snack or a light lunch.
The post Zucchini Chips With Black Bean Salsa appeared first on MyFitnessPal Blog.
from MyFitnessPal Blog https://blog.myfitnesspal.com/watch/zucchini-chips-with-black-bean-salsa/
via IFTTT
Zucchini Chips With Black Bean Salsa
Most people might not guess that pills (or creams, patches, and inhalers, for that matter) have a big impact on the environment — but they do.
Climate change is leading to noticeable effects on the environment, as well as to consequences for our health, such as rising rates of asthma and new patterns of infectious diseases. The key driver of climate change is greenhouse gas emissions. Our health care system plays a large role, contributing close to 10% of our nation’s greenhouse gases. The US is also responsible for more than 25% of the world’s total health care emissions.
Within our health care system, pharmaceutical drugs and chemicals are the largest line-item contributor to greenhouse gas emissions. In addition, pharmaceutical waste throughout the global supply chain can lead to environmental and animal toxicities, and in the case of antibiotic residues, to antimicrobial resistance (aka “superbugs”). In 2018, 5.8 billion prescriptions were filled in the US. Meanwhile, consumers spent $34 billion on over-the counter medications.
Many of these drugs are lifesaving, offering us enormous benefits and healthier lives when taken correctly. But with some thought, there may be a few things you can do to make your medicine cabinet more environmentally friendly, while still keeping your health front and center.
Minimize waste when buying medicines
Less is more. Filling 90-day supplies of medications can reduce the overall cost per pill, offer more convenience, and require less packaging. But in some situations, it makes sense to request smaller quantities, such as when you are trying a new medicine, or buying over-the-counter medications that you use infrequently and do not expect to finish before the expiration date.
Do the math. If your doctor is recommending a dose change and the math works out, consider halving or doubling your current pills first. If this is working, you can then request a prescription for the new dose strength for your next refill.
Fill it when you use it. Don’t pick up a prescription unless you are going to use it, except for an emergency medicine you should have on hand. If you are given the option of getting a medication to take if your symptoms get worse or don’t improve, ask your doctor to send the prescription to the pharmacy, and notify the pharmacy that you will let them know if you want it filled.
Downsizing your medicine cabinet
Review the benefits versus harms. Bring all your prescription and over-the-counter medications to your appointments, and periodically review them with your primary care doctor. Make sure your drug regimen offers more benefits than harms for your situation. This is especially helpful if you see a lot of different doctors who prescribe medications for you. Sometimes, people stumble into a cascade, where one drug is added to treat symptoms that are side effects of another. But be sure to discuss with your doctor before making any changes; it may be harmful to stop some medications, and others may need to be tapered slowly.
Incorporate lifestyle medicine. Talk to your doctor about lifestyle medicine, which focuses on healthy habits like regular exercise and healthful foods to prevent disease and promote longevity. Often, these lifestyle changes can help reduce or eliminate the need for medications.
Inhalers: Know your options
Explore options. If you have asthma or chronic obstructive pulmonary disease (COPD), ask your doctor what your options are for inhalers. Metered dose inhalers (MDIs) use hydrofloroalkane propellants, which are greenhouse gases, to deliver the medication. Check if there is an equivalent dry powder inhaler (DPI) option for you. However, not everyone can use DPIs, which rely on patients to take quick deep breaths to draw the medication into the lungs. (For this reason, rescue inhalers used during an asthma attack are usually MDIs.) Your inhaler choices will also depend on cost and coverage from your insurer. In the end, the important thing is to use the inhaler device that works best for you in controlling your condition.
Proper disposal of medicines
Know when to flush. Do not put medications down the toilet or sink (unless they’re on the FDA flush list), as this may contaminate lakes, rivers, agriculture, and drinking water. Read the packages for any drug disposal instructions. Many pharmacies or local public safety agencies like the police will accept unused medications and dispose of them safely. National Prescription Drug Take Back Day is April 24, 2021 so check for safe collection sites near you.
Some medicines can be discarded in trash. Remove personal identifying labels first, and then mix the medication in a container with coffee grounds, cat litter, or soil. (This is not recommended for controlled substances like opioids and other addictive medicines.) Visit this FDA web page for more information about drug disposal.
Health care is a partnership, and with thought and care, we can work together to have the best of both worlds — a healthier you, and a healthier planet.
The post Pills and the planet: Environmentally-friendly steps for your medicine cabinet appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/pills-and-the-planet-evironmentally-friendly-steps-for-your-medicine-cabinet-2021042222442
via IFTTT
Pills and the planet: Environmentally-friendly steps for your medicine cabinet
Wednesday, 21 April 2021
There is growing interest in the human body’s microbiome and its connection to chronic disease. A new study examines that connection, along with how the foods we eat influence the composition of our microbiome.
Microbiome protects host and plays role in disease risk
The microbiome consists of the genes of tiny organisms (bacteria, viruses, and other microbes) found in the gastrointestinal tract, primarily in the small and large intestine. The normal gut flora — another term for the microbiome — protects its human host. For the microbiome to flourish, the right balance must exist, with the healthy species dominating the less healthy.
Scientists do not fully understand how the microbiome factors into the risk of developing chronic diseases, such as heart disease, obesity, and type 2 diabetes. Many factors, including differences between individuals and individual diets, have made this a difficult area to investigate.
Study investigates relationships between diet, microbiome, and disease risk
But a new study, published in Nature Medicine, accounts for these factors and sheds light on how our diets shape our microbiome and how our microbiome, in turn, influences our disease risk.
The researchers studied more than 1,100 individuals enrolled in PREDICT 1, a large trial looking at individual responses to food. They used a technique called metagenomic sequencing to identify, classify, measure, and analyze genetic material from the study participants’ microbiomes. They also collected detailed, long-term dietary intake information from all of these individuals, so they could analyze their dietary patterns, including their intake of different food groups, foods, and nutrients. In addition, they collected information from the study participants on a variety of factors that are known to influence metabolism and disease risk, including pre- and post-meal measures of blood sugar (glucose), cholesterol, and inflammation. Finally, they measured personal health attributes of the study participants, including age, weight, body mass index (BMI), body fat, and blood pressure.
Diet influences microbiome and microbiome influences disease risk
The study found that the health of the microbiome is influenced by diet, and that the composition of the microbiome influences the risk of health outcomes. The results showed that specific gut microbes were associated with specific nutrients, foods, food groups, and overall diet composition. Health conditions such as heart disease, type 2 diabetes, obesity, and general inflammation appeared to be most impacted by diet-influenced changes to the microbiome.
For example, less healthy dietary patterns (dairy desserts, unhealthy meats, processed foods) supported gut species that were associated with measures of blood sugar, cholesterol, and inflammation that are significantly associated with higher risk of cardiac events, strokes, and type 2 diabetes.
In contrast, a more diverse gut microbiome was tied to healthy dietary patterns (high-fiber vegetables like spinach and broccoli, nuts, and, heathy animal foods such as fish and eggs) and was linked to measurements tied to lower risk of certain chronic diseases. In addition, the study found that polyunsaturated fats (found in fish, walnuts, pumpkin, flax and chia seeds, sunflower, safflower, and unhydrogenated soybean oils) produce healthy gut species linked to a reduced risk of chronic disease.
Minimally processed, plant-based diet is good for the microbiome and for reducing disease risk
So what do these findings mean for us? First, the study showed that eating more unprocessed plant foods — fruits, vegetables, nuts, seeds, and whole grains — allows the gut microbiome to thrive. Some animal foods, such as fish and eggs, are also favorable. Avoiding certain animal foods, such as red meat and bacon, dairy foods, and highly processed foods (even processed plant foods such as sauces, baked beans, juices, or sugar-sweetened drinks and desserts) prevents less-healthy gut species from colonizing the gut.
It is important to note that food quality matters; processed or ultra-processed plant-based foods were not associated with heathy clusters of gut microbes. When choosing foods, consider whether they are processed or unprocessed, in addition to whether they are a plant or animal food.
It can also be helpful to think in terms of dietary patterns, rather than individual foods or food groups. Meal patterns that emphasize foods beneficial to the microbiome are the whole-food, plant-based dietary patterns. These include vegan (no animal products) and ovo-vegetarian (vegetarian plus eggs) diets. The pescatarian eating pattern, in which oily and white fish are the meats of choice, is also good for the microbiome.
Emphasizing minimally processed plant foods allows the gut microbiome to thrive, providing protection against, or decreasing the risk of, chronic diseases such as heart disease, diabetes, metabolic disease, and obesity.
The post Diet, disease, and the microbiome appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/diet-disease-and-the-microbiome-2021042122400
via IFTTT
Diet, disease, and the microbiome
Tuesday, 20 April 2021
Did the print on that label suddenly shrink? If you’re in your 40s or beyond, you may have asked yourself that question as you struggled to read something that you used to be able to see clearly with no problem.
Blame your aging eyes. Much like our joints, our eyes undergo age-related changes. While eye problems can affect people of any age, some conditions become more common after age 40.
Getting older? Three common eye conditions
Presbyopia. The lens of the eye gets stiffer with age, which makes it harder to focus on objects nearby — hence your label-reading struggles. Many people find satisfaction with inexpensive reading glasses, but once you need them, it’s time for a midlife vision check-up.
Cataracts. Another common condition that can crop up as you age is cataracts, a clouding of the lens of your eye that can impair vision. Cataracts affect about half of people ages 65 to 74. Treatment typically involves an outpatient surgical procedure to replaces the clouded lens.
Dry eye syndrome. This condition affects more than 15 million adults in the United States, and occurs due to a reduction in tear production. With less natural lubrication your eyes can become irritated, sticky, or you may feel a burning or scratchy sensation in the eye. Depending on severity, symptoms can be treated using eye drops that simulate your natural tears, a topical prescription drug, or a device to increase tear production.
Additional eye conditions that may occur with age or illness
Posterior vitreous detachment (PVD). Signs of this condition include visual disruptions, such as seeing light streaks, floaters, or a cobweb-like haze. These occur because the jelly-like substance called vitreous in the eye starts to liquefy and shrink, causing it tug on the retina.
Call your medical team right away if you notice these signs. While most people experiencing PVD won’t need treatment, in some cases the vitreous can completely detach from or tear the retina. A tear or detachment can cause vision loss, and requires a laser procedure or surgery to repair the problem, according to the American Society of Retina Specialists.
Glaucoma. Another condition that becomes more common after age 40 is glaucoma. This painless, often symptomless condition damages the optic nerve that transmits information from your eyes to your brain. When not treated, glaucoma can lead to peripheral or central vision loss. Most often, glaucoma is treated with prescription eye drops designed to reduce the pressure in your eye. Less commonly, your doctor may recommend a laser procedure or surgery.
Age-related macular degeneration (AMD). This condition causes degeneration of the retina, a thin layer of tissue at the back of the eye. Light-sensitive cells of the retina capture images and transmit them to the brain through the optic nerve. AMD affects a central part of the retina called the macula. It can lead to blurred or distorted vision, and possibly a blind spot in a person’s field of vision. Treatment, which may include medication or laser therapy, can often help prevent or at least delay vision loss.
Diabetic retinopathy. This condition also causes damage to the retina. For people with diabetes, keeping blood sugar and blood pressure under control helps prevent diabetic retinopathy. If it is detected, your eye specialist will recommend treatment, usually eye injections or laser therapy.
Easy ways to maintain eye health
Many eye conditions can be effectively treated to protect your vision if they are caught early. That’s why it’s wise to get regular eye exams, to spot potential problems and address them before they affect your eyesight.
You can also take other steps to ensure that your eyes stay healthy, such as exercising, eating a healthy diet, quitting smoking, and protecting your eyes from ultraviolet rays by wearing sunglasses outside.
The post Want healthy eyes? What to know at 40 and beyond appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/want-healthy-eyes-what-to-know-at-40-and-beyond-2021042022436
via IFTTT
Want healthy eyes? What to know at 40 and beyond
Monday, 19 April 2021
Doctors told you that your COVID-19 virus infection cleared months ago. However, even though you no longer struggle to breathe, and your oxygen levels have returned to normal, something doesn’t feel right. In addition to constant headaches, you find yourself struggling with seemingly easy tasks. The fatigue you experience makes moving from the bed to the kitchen feel like an accomplishment. But most troubling for you is a feeling of dread, a nervousness so severe you can feel your heart pounding. Constant worries now keep you from sleeping at night.
What are the mental health effects of COVID-19?
We are still learning about the long-term effects of COVID-19 on the brain. Data from Wuhan suggest that the virus may invade the brain, with more than one-third of infected patients developing neurologic symptoms. In addition to brain infection, we know that the pandemic has resulted in worsening mental health outcomes due to the psychological toll of isolation, loneliness, unemployment, financial stressors, and the loss of loved ones. The prescription of antidepressants has spiked, intimate partner violence has increased, and suicidal thoughts are on the rise, especially in young adults.
Does COVID-19 infection increase the risk of psychiatric disorders?
Until recently, mental health outcomes as a result of COVID-19 infection were not known. A new study of electronic health records of 69 million people found that COVID-19 infection increased the risk of developing a psychiatric disorder, dementia, or insomnia. Furthermore, people with psychiatric disorders were 65% more likely to be diagnosed with COVID-19, which may be related to behavioral factors, lifestyle factors (such as smoking), inflammation, or psychiatric medication. This is the first large study to show that infection with COVID-19 indeed increases the risk of developing psychiatric disorders.
The long-term mental health effects of COVID-19 infection remain to be seen. Following the influenza pandemic of 1918–19, offspring of mothers infected during pregnancy were found to have higher rates of schizophrenia. It is thought that virus infection during pregnancy may be one risk factor for the development of mental illness related to the body’s immune response. If COVID-19 infection even slightly increases the risk of mental illness in offspring, this could have a large effect at the population level, given the high numbers of infections worldwide.
Do you have a psychiatric disorder as a result of COVID-19?
You may feel fatigued, stressed, or sad due to the effects of COVID-19 on your body, or due to life circumstances. However, even if you screen positive for depression or anxiety at your doctor’s visit, remember that screening tools are not diagnostic. People with physical symptoms of COVID-19 infection often screen positive for depression, as symptoms of infection often overlap with symptoms of depression. For example, poor sleep, impaired concentration, and reduced appetite may be due to a medical illness rather than depression.
For a doctor to make an accurate diagnosis, you may need to wait a period of time to monitor symptom development. Although antidepressants are often prescribed for mood and anxiety disorders, keep in mind that mild to moderate symptoms often go away on their own when life circumstances improve. If this is your first episode of depression or your first experience of anxiety, you may not require specialist treatment if your symptoms are mild. If you do start a medication, make sure to regularly review your treatment with your doctor and make changes as needed.
What steps can you take to minimize the mental health consequences of COVID-19 infection?
- Get vaccinated. This is especially important for people with psychiatric disorders, which are independent risk factors for COVID-19 infection.
- Continue to wear a mask and physically distance. However, aim to maintain social connections.
- Make use of resources. Online therapies, workbooks, and mobile applications (COVID coach, CBT-I coach) can provide benefits without risking exposure during treatment.
- Advocate for others. COVID-19 long haulers may not be in the position to advocate for workplace modifications, life insurance, or mental health coverage, especially if suffering from fatigue and brain fog.
- Perform physical activity. in addition to being as effective as medications on mood and anxiety, physical activity also helps with memory and heart health.
- Make use of relaxing rituals. When the world seems out of control, try establishing a ritual. Having control over even one part of your day can help you feel grounded.
- Use caution with sleep aids and as-needed medications. Short-term use can quickly become long-term use, leading to medication tolerance, dependence, and rebound anxiety.
- Limit alcohol and cannabis use. Prolonged stress from caring for sick loved ones, unemployment, increased time at home, and relationship stressors can result in increased and problematic substance use.
- Be mindful of caffeine. If post-COVID fatigue is severe, discuss other options with your doctor, as excess caffeine can exacerbate anxiety and sleep problems.
- Check in and ask how you can help your loved ones, friends, colleagues, and neighbors. It is often much easier to turn down help than to ask for help. If someone is privately struggling with thoughts of suicide, a simple check-in call or kind gesture can be lifesaving. The National Suicide Prevention Lifeline (800-273-8255) is available to anyone in severe distress.
The post Could COVID-19 infection be responsible for your depressed mood or anxiety? appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/could-covid-19-infection-be-responsible-for-your-depressed-mood-or-anxiety-2021041922391
via IFTTT
Could COVID-19 infection be responsible for your depressed mood or anxiety?
Friday, 16 April 2021

This lighter version subs in hearty lentils & mushrooms for 1/2 the ground beef. So flavorful, you won’t miss the extra meat!
The post Meat-Lite Meatloaf appeared first on MyFitnessPal Blog.
from MyFitnessPal Blog https://blog.myfitnesspal.com/watch/meat-lite-meatloaf/
via IFTTT
Meat-Lite Meatloaf
Did you know that antidepressant medications are often prescribed for people without depression?
It’s true. Antidepressants are frequently prescribed for chronic pain, especially pain related to nerve disease (called neuropathic pain), chronic low back or neck pain, and certain types of arthritis.
In fact, some guidelines for the treatment of chronic low back pain and osteoarthritis (the most common type of arthritis) include antidepressants. One antidepressant in particular, duloxetine (Cymbalta), is FDA-approved for these conditions.
Just how antidepressants reduce pain is not well understood. One possibility is they affect chemicals in the brain involved in pain perception, a mechanism that differs from how they fight depression.
Not usually the first choice for pain relief
For people with chronic low back or neck pain or osteoarthritis of the hip or knee, an antidepressant medication is not usually the first treatment recommended. Other approaches, such as physical therapy, exercise, losing excess weight, nonsteroidal anti-inflammatory drugs (NSAIDs), or cortisone injections are usually tried first. But if these aren’t helpful, antidepressants such as duloxetine or amitriptyline might be a reasonable next step.
When prescribed for pain, the initial dose is typically low (often lower than the starting dose for depression). It’s gradually increased if necessary. Ideally, people notice a benefit within weeks of starting the drug, and the medication can be continued at the lowest effective dose. Switching to a different antidepressant may be recommended if pain is not well controlled, side effects develop, or there is an interaction with another medication.
A new study suggests antidepressants don’t work well for common types of pain
Past research on antidepressants for chronic pain, such as duloxetine for osteoarthritis of the knee, amitriptyline or duloxetine for chronic low back pain, and amitriptyline for chronic neck pain, demonstrated modest, short-term benefit. But the studies were limited: most trials were small and lasted only a few months or less. Notably, medication side effects, such as nausea, constipation, and erectile dysfunction, were common in these trials.
Now a 2021 study has combined the data from past research to get a better sense of just how safe and effective antidepressants are for these conditions. The news isn’t good:
- On average, treatment with antidepressants minimally reduced pain and disability compared with placebo. The improvement in pain — about 4 points on a scale of 0 to 100 — was considered too small to be noticeable.
- People treated with certain antidepressants for chronic pain often stopped taking the medication because it didn’t work, caused unacceptable side effects, or both.
- People with both chronic pain and depression did not experience more improvement than people with chronic pain alone.
Sciatica may be an exception: antidepressants may have reduced pain for up to a year. However, the quality of the prior research was poor, so the study authors were not confident about these conclusions.
These findings cast doubt on the usefulness of antidepressant treatment for these common causes of chronic pain. However, they don’t rule out the possibility that some individuals may get more relief from these medications than others.
The bottom line
The available evidence suggests that, on average, the benefit of antidepressants for osteoarthritis or chronic low back pain and neck pain is modest at best, and tends to be temporary. That’s disappointing because, for many pain sufferers, there are no reliably effective treatments (short of joint replacement for osteoarthritis).
So, if you’re on an antidepressant for pain and you aren’t sure if it’s working, talk to your doctor about whether you should consider stopping it. But don’t stop it on your own. There may be other reasons your doctor is recommending this medication, and many antidepressants should be gradually reduced, not stopped all at once, to avoid discontinuation symptoms.
If you’re taking an antidepressant for pain, it’s worth revisiting whether it’s really doing anything for you and whether it might be time to shorten your medication list. Not only might you simplify your medical regimen, you may also reduce the cost of your medicines and the risk of medication-related side effects.
Follow me on Twitter @RobShmerling
The post Are antidepressants also pain relievers? appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/are-antidepressants-also-pain-relievers-2021041622383
via IFTTT
Are antidepressants also pain relievers?
Thursday, 15 April 2021
Like the rest of the country, I awoke on Wednesday, March 17 to the horrific news of a mass shooting in Atlanta that killed eight people. Six were Asian women, ranging in age from 44 to 74. I immediately went numb. Lulu Wang, the Chinese American filmmaker and director of The Farewell, gave voice to my pain on social media: “I know these women. The ones working themselves to the bone to send their kids to school, to send money back home.”
The fact is, I’ve been in a state of numbness for much of the past year. On top of the unprecedented strains that COVID-19 has placed on all of us, Asian Americans like me have had to confront skyrocketing rates of discrimination, verbal assaults, and physical violence. We have been punched, shoved, stabbed, spat at, told that the pandemic is our fault, we brought it this country, and we should go back to wherever we came from. Our most vulnerable — women, youth, and the elderly — are disproportionately targeted.
Racial trauma and fear in the news
The relentless drumbeat of headlines and viral videos depicting unprovoked violence against Asian Americans contributes to vicarious trauma, even for those not directly attacked. Fearful for the safety of my parents, both in their 70s in Virginia, I called home last March to warn them not to go outside too much, to always shop in daylight, to be very careful. My heart broke then thinking about their deeply held belief in the goodness and possibility of this country, which motivated their immigration here almost 50 years ago. And it broke again two weeks ago when my mother told me a teen had yelled a racial slur at her.
As a psychiatrist and director of the nonprofit, volunteer-operated MGH Center for Cross-Cultural Student Emotional Wellness, I am very aware that Asian Americans grappled with mental health issues long before COVID-19. We’ve been stereotyped since the 1960s as the “Model Minority”: a uniformly successful group that keeps its mouth shut and doesn’t rock the boat. That stereotype intersects neatly with cultural values prizing stoicism and self-sacrifice, and greatly stigmatizing anything perceived as shameful — including mental health struggles. Asian Americans are two to three times less likely than whites to seek mental health treatment, and more likely to find available services unhelpful. Our research shows that Asian American and Pacific Islander (AAPI) college students are about half as likely as white students to carry a psychiatric diagnosis such as anxiety or depression — possibly because they have never seen a mental health professional — but almost 40% more likely to have attempted suicide.
To that burden we now add racial trauma — the mental and emotional injury caused by race-based discrimination. As described by psychologist Robert Carter, racial trauma makes the world feel less safe, and lingers in the psyche long after the incident is over. Victims report anxiety, hypervigilance (a state of increased alertness), avoidance of situations that remind them of the attack, poor sleep, mood swings, and yes, numbness. These symptoms mirror those of post-traumatic stress disorder. Words actually can and do hurt us, contrary to a childhood rhyme — sometimes even more than sticks and stones.
The weight of racism, past and present
Time and again, events of this pandemic have driven home that being a Model Minority is not enough — AAPI doctors and nurses have been assaulted, even by patients they were caring for. What I never learned, either from my parents while growing up or from my high school history curriculum, is that anti-Asian racism is nothing new; it is woven into the very fabric of this country.
Looking back teaches us much. Fear of Chinese laborers taking American jobs in the mid-1800s fanned persecution and caricaturing of Chinese and Asians as the “Yellow Peril,” diseased, lewd, and treacherous. In 1871, a 500-person mob slaughtered, mutilated, and hung 20 Chinese men in Los Angeles during one of the deadliest lynching incidents in US history. The Chinese Exclusion Act of 1882 was the only law to prohibit a specific ethnic or national group from immigrating to the US and naturalizing as citizens. During World War II, President Franklin D. Roosevelt signed an executive order forcing more than 120,000 Japanese Americans into internment camps — over 60% of whom were US citizens. The hatred we see now echoes these earlier refrains of Asians as diseased invaders and disloyal, perpetual foreigners.
A different perspective on the Model Minority myth
I now see the Model Minority label in a different light. Who could blame Asian Americans for embracing a seemingly more positive reputation, given the pervasive discrimination they faced? But that stereotype is both damaging and wrong. It obscures the significant disparities and challenges faced by the extraordinarily diverse AAPI community, which has the greatest income inequality of any racial group in the US. And it encourages policymakers to overlook our issues. Most insidiously, it sets up a divisive contrast with other minorities, blaming them for their problems and perpetuating the fiction that structural racism does not exist. On top of all that, we now see how quickly the stereotype of the Model Minority reverts to the Yellow Peril.
Will the racism we’ve experienced during this pandemic be a turning point in our community’s racial awakening? Our Center can attest to a new hunger among AAPI parents for education and resources to help them talk to their kids about race and racism. More members of our community are organizing, becoming politically active, and speaking out about incidents of hate that previously went unreported. It’s long past time that we break our silence and speak out against AAPI hate, yes, but also that we stand proudly in solidarity with other marginalized groups against violence and oppression in all its forms.
Resources
- MGH Center for Cross-Cultural Student Emotional Wellness. Resources on anti-Asian racism and mental health, with sections dedicated to parents, students, therapists, educators, and allies.
- Toolkit to help Asian parents talk to teens about racism (available in five languages).
- Report incidents of anti-Asian hate at Stop AAPI Hate.
The post Anti-Asian racism: Breaking through stereotypes and silence appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/anti-asian-racism-breaking-through-stereotypes-and-silence-2021041522414
via IFTTT
Anti-Asian racism: Breaking through stereotypes and silence
Breast cancer remains the most common cancer among women. In the last two decades, the treatment of breast cancers has become personalized. This has been possible due to the subtyping of breast cancers. Breast cancers have been subtyped based on the receptors on the breast cancer cell. The most clinically significant receptors — those that have targeted therapies — are the estrogen and progesterone receptors and the human epidermal growth factor receptor 2 (HER2). Cancers that have the estrogen and progesterone receptors are termed hormone receptor (HR)-positive cancers.
The development of hormone therapy for HR-positive breast cancers means that some women, for whom the risks of chemotherapy outweigh the benefits, may be able to forego chemotherapy. The development of genomic assays, tests that analyze genes expressed in cancer, have provided a way to help doctors and women decide who will obtain the most benefit from chemotherapy.
How does genomic testing help to personalize breast cancer treatment?
Increasingly detailed knowledge about breast cancers has led to the development of personalized therapy. In addition to knowing the type and stage of your cancer, genomic testing has further refined how we assess the risk of recurrence for breast cancer. One genomic test, Oncotype Dx, is a useful tool that can help predict the likelihood of benefit from chemotherapy, as well as the risk of recurrence for invasive breast cancer.
Not all women will require chemotherapy, but for some women hormone therapy alone is not enough. Oncotype Dx analyzes the expression of 21 genes in HR-positive, HER2-negative breast cancer and assigns a recurrence score (RS) based on risk of recurrence. The Oncotype Dx test places women into three groups: low, intermediate or moderate, and high risk of recurrence. Women with a low score do not need chemotherapy and benefit the most from hormone therapy, while women who have a high recurrence score benefit the most from chemotherapy in addition to hormone therapy.
There is new research to help women make decisions about chemotherapy
Until recently, it was unclear how much benefit women with an intermediate risk score obtained from chemotherapy. A randomized clinical controlled trial, the Tailor Rx trial, answered this question. The trial randomized women with node-negative (cancer that has not yet spread to the lymph nodes), HR-positive, HER2-negative breast cancers with an intermediate risk score to hormone therapy alone, or to chemotherapy in additional to hormone therapy. The results showed that most women with an intermediate risk of invasive cancer did not get any added benefit with chemotherapy. However, the subgroup of women who did benefit from chemotherapy were premenopausal women under age 50.
While the results of the Tailor Rx trial were practice-changing, it did lead to questions about the benefit of chemotherapy in women whose cancer has spread to their lymph nodes and who had HR-positive, HER2-negative breast cancer. The RxPonder trial answered this question.
The RxPonder trial randomized 5,015 women with stage II/III HR-positive, HER2-negative breast cancer, with one to three positive lymph nodes, and an intermediate RS (≤ 25). Patients were randomized to receive hormone therapy alone, or hormone therapy with chemotherapy. The main goal of the study was to determine how many women did not get a recurrence of the invasive breast cancer while they were being followed.
There were many ways to compare the women in the study, but the main characteristics chosen for comparison were: menopausal status, RS, and the kind of axillary surgery they received. At a median follow up of 5.1 years, there was no association between chemotherapy benefit and RS value between zero and 25 for the entire population. However, there was an association seen between chemotherapy benefit and menopausal status. This trial provided evidence that even women with cancer in their lymph nodes, if they had a low or intermediate RS, could avoid chemotherapy.
Premenopausal women responded better to hormone therapy and chemotherapy
Of the women enrolled in the RxPonder trial, 3,350 were postmenopausal and 1,665 were premenopausal. Further analysis by menopausal status revealed that there was no difference in five-year survival for postmenopausal women treated with hormone therapy alone versus hormone therapy with chemotherapy.
However, for premenopausal women there was a 46% reduction in the risk of invasive disease. For this subgroup of women, the five-year, invasive disease-free survival rates were 94.2% in women treated with hormone therapy and chemotherapy, compared to 89% in women treated with hormone therapy alone. The premenopausal women who received both chemotherapy and hormone therapy had an additional benefit of around 5%. It is unclear if the survival benefit seen in premenopausal women is primarily due to chemotherapy’s effect, or indirectly by ovarian suppression due to chemotherapy
What does this mean for breast cancer treatment decision-making?
The treatment of breast cancer has truly become personalized. It has always been important to know the stage of your caner, but now it is also important to know the type of your cancer. With this information, women can make an informed discussion with their oncologist about the risks and benefits of chemotherapy.
If you are a premenopausal woman with a HR-positive, node-positive breast cancer, chemotherapy and hormone therapy may give you the greatest chance of decreasing your risk of the cancer coming back. However, for a postmenopausal woman with HR-positive breast cancer, chemotherapy may not add many treatment benefits to hormone therapy, and it carries risks that may affect your quality of life. Studies like the TailorRx and RxPonder trials have provided more information to help you make an informed decision.
The post Can some postmenopausal women with breast cancer skip chemotherapy? appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/can-some-postmenopausal-women-with-breast-cancer-skip-chemotherapy-2021041522344
via IFTTT
Can some postmenopausal women with breast cancer skip chemotherapy?
Are you stressed out? Your skin can show it. Studies show that both acute and chronic stress can exert negative effects on overall skin wellness, as well as exacerbate a number of skin conditions, including psoriasis, eczema, acne, and hair loss.
But it’s not just a one-way street. Research has also shown that skin and hair follicles contain complex mechanisms to produce their own stress-inducing signals, which can travel to the brain and perpetuate the stress response.
Stress and the two-way street between your brain and skin
You may already have experienced the connection between the brain and skin. Have you ever gotten so nervous that you started to flush or sweat? If so, you experienced an acute, temporary stress response. But science suggests that repeated exposure to psychological or environmental stressors can have lasting effects on your skin that go far beyond flushing — and could even negatively affect your overall well-being.
The brain-skin axis is an interconnected, bidirectional pathway that can translate psychological stress from the brain to the skin and vice versa. Stress triggers the hypothalamus-pituitary-adrenal (HPA) axis, a trio of glands that play key roles in the body’s response to stress. This can cause production of local pro-inflammatory factors, such as cortisol and key hormones in the fight-or-flight stress response called catecholamines, which can direct immune cells from the bloodstream into the skin or stimulate pro-inflammatory skin cells. Mast cells are a key type of pro-inflammatory skin cell in the brain-skin axis; they respond to the hormone cortisol through receptor signaling, and directly contribute to a number of skin conditions, including itch.
Because the skin is constantly exposed to the outside world, it is more susceptible to environmental stressors than any other organ, and can produce stress hormones in response to them. For example, the skin produces stress hormones in response to ultraviolet light and temperature, and sends those signals back to the brain. Thus, psychological stressors can contribute to stressed-out skin, and environmental stressors, via the skin, can contribute to psychological stress, perpetuating the stress cycle.
How else can stress affect your skin?
Psychological stress can also disrupt the epidermal barrier — the top of layer of the skin that locks in moisture and protects us from harmful microbes — and prolong its repair, according to clinical studies in healthy people. An intact epidermal barrier is essential for healthy skin; when disrupted, it can lead to irritated skin, as well as chronic skin conditions including eczema, psoriasis, or wounds. Psychosocial stress has been directly linked to exacerbation of these conditions in small observational studies. Acne flares have also been linked to stress, although the understanding of this relationship is still evolving.
The negative effects of stress have also been demonstrated in hair. One type of diffuse hair loss, known as telogen effluvium, can be triggered by psychosocial stress, which can inhibit the hair growth phase. Stress has also been linked to hair graying in studies of mice. The research showed that artificial stress stimulated the release of norepinephrine (a type of catecholamine), which depleted pigment-producing stem cells within the hair follicle, resulting in graying.
How can you manage stress skin?
While reducing stress levels should theoretically help to alleviate damaging effects on the skin, there’s only limited data regarding the effectiveness of stress-reducing interventions. There is some evidence that meditation may lower overall catecholamine levels in people who do it regularly. Similarly, meditation and relaxation techniques have been shown to help psoriasis. More studies are needed to show the benefit of these techniques in other skin conditions. Healthy lifestyle habits, including a well-balanced diet and exercise, may also help to regulate stress hormones in the body, which should in turn have positive effects for skin and hair.
If you are experiencing a skin condition related to stress, see a dermatologist for your condition, and try some stress-reducing techniques at home.
The post Stress may be getting to your skin, but it’s not a one-way street appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/stress-may-be-getting-to-your-skin-but-its-not-a-one-way-street-2021041422334
via IFTTT
Stress may be getting to your skin, but it’s not a one-way street
Tuesday, 13 April 2021
If you’ve been stuck mostly at home with one or more family members over the past year, chances are you’ve gotten on one another’s nerves occasionally. When you’re under a lot of stress, it’s not uncommon say something unkind, or even to lash out in anger to someone you care about. And we all make thoughtless mistakes from time to time, like forgetting a promise or breaking something.
Not sure if you should apologize?
Even if you don’t think what you said or did was so bad, or believe that the other person is actually in the wrong, it’s still important to apologize when you’ve hurt or angered someone. “To preserve or re-establish connections with other people, you have to let go of concerns about right and wrong and try instead to understand the other person’s experience,” says Dr. Ronald Siegel, assistant professor of psychology at Harvard Medical School. That ability is one of the cornerstones of emotional intelligence, which underlies healthy, productive relationships of all types.
How to apologize genuinely
For an apology to be effective, it has to be genuine. A successful apology validates that the other person felt offended, and acknowledges responsibility (you accept that your actions caused the other person pain). You want to convey that you truly feel sorry and care about the person who was hurt, and promise to make amends, including by taking steps to avoid similar mishaps going forward as in the examples below.
According to the late psychiatrist Dr. Aaron Lazare, an apology expert and former chancellor and dean of the University of Massachusetts Medical School, a good apology has four elements:
- Acknowledge the offense. Take responsibility for the offense, whether it was a physical or psychological harm, and confirm that your behavior was not acceptable. Avoid using vague or evasive language, or wording an apology in a way that minimizes the offense or questions whether the victim was really hurt.
- Explain what happened. The challenge here is to explain how the offense occurred without excusing it. In fact, sometimes the best strategy is to say there is no excuse.
- Express remorse. If you regret the error or feel ashamed or humiliated, say so: this is all part of expressing sincere remorse.
- Offer to make amends. For example, if you have damaged someone’s property, have it repaired or replace it. When the offense has hurt someone’s feelings, acknowledge the pain and promise to try to be more sensitive in the future.
Making a heartfelt apology
The words you choose for your apology count. Here are some examples of good and bad apologies.
| EFFECTIVE WORDING | WHY IT WORKS |
| “I’m sorry I lost my temper last night. I’ve been under a lot of pressure at work, but that’s no excuse for my behavior. I love you and will try harder not to take my frustrations out on you.” | Takes responsibility, explains but does not excuse why the mistake happened, expresses remorse and caring, and promises reparation. |
| “I forgot. I apologize for this mistake. It shouldn’t have happened. What can I do to avoid this problem in the future?” | Takes responsibility, describes the mistake, makes the person feel cared for, and begins a conversation about how to remedy the error. |
| INEFFECTIVE WORDING | WHY IT WON’T WORK |
| “I apologize for whatever happened.” | Language is vague; offense isn’t specified. |
| “Mistakes were made.” | Use of passive voice avoids taking responsibility. |
| “Okay, I apologize. I didn’t know this was such a sensitive issue for you.” | Sounds grudging, thrusts the blame back on to the offended person (for “sensitivity”). |
The post The art of a heartfelt apology appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/the-art-of-a-heartfelt-apology-2021041322366
via IFTTT
The art of a heartfelt apology
Monday, 12 April 2021
Myasthenia gravis (MG) — a medical term that translates as “serious muscle weakness” — is a rare neuromuscular disease. An estimated 30,000 to 60,000 people in the United States have this disorder, which affects people of all ages, sexes, and ethnicities. Recently updated consensus guidelines have added to our knowledge of different forms of myasthenia gravis and improved approaches to treatment.
What are the symptoms of myasthenia gravis?
Myasthenia gravis impairs the transmission of signals from nerves to muscles at a site called the neuromuscular junction (NMJ), where nerves make contact with muscle. This causes temporary weakness of muscles in use. When the affected muscle or muscle group is rested, it recovers strength.
Throughout the day, your body uses many muscle groups repeatedly; this is true even if you’re not especially active. Because myasthenia gravis is marked by use-related weakness in particular muscle groups, repeated activity of affected muscle makes weakness worse. The weakness improves with rest, only to recur as activity resumes.
Which muscle groups are affected may vary from person to person. Often, the muscles around the eyes are affected. Drooping of the eyelids and double vision are common symptoms. People may complain that they are fine when they wake up, but as the day goes on, their eyelids droop. After a nap, their eyes are wide open. They could start out seeing just fine when driving, but as they drive on they develop double vision. They cannot eat a whole bagel because their jaw gets tired after a while, although they can eat pasta without a problem. Their arms get tired halfway through blow-drying their hair and they have to stop, put their arms down for a while, and then go on.
What causes myasthenia gravis?
Several disorders and even some medications can affect the neuromuscular junction. I’ll focus here on a form of myasthenia gravis called autoimmune MG. If you have autoimmune MG, your immune system produces antibodies that inappropriately attack certain proteins at the junction. One such protein is the acetylcholine receptor (AchR), located on the muscle membrane at the junction.
This particular protein binds to a chemical messenger called acetylcholine (Ach). Ach is released by the nerve terminal when an electrical signal reaches it, causing a muscle to contract. But AchR antibodies destroy and reduce the number of AchR, so that the transmission of impulses from nerve to muscle is impaired and muscle weakness results.
Antibodies may also be directed against other important proteins at the neuromuscular junction that would normally help to maintain AchR proteins, causing the same end result. Two such proteins that may be targeted by antibodies are muscle-specific kinase (MuSK) and lipoprotein-related protein 4 (LRP-4).
How is myasthenia gravis treated?
Treatment is directed first toward improving symptoms. The drug most commonly used is pyridostigmine. Pyridostigmine prolongs the time that Ach stays in the neuromuscular junction, thus giving it more of a chance to bind to the reduced number of AchR receptors.
Additionally, people with autoimmune MG receive treatment to suppress the abnormal immune response underlying the disease. Many approaches are used to achieve this.
In 2016, the Myasthenia Gravis Foundation of America (MGFA) convened an international task force of neuromuscular specialists to develop guidance around treatment. This panel updated that guidance in 2020, adding new recommendations for a surgical procedure called thymectomy; treating ocular MG (MG confined to the muscles around the eyes); and the use of three medications to address abnormal immune response: methotrexate, rituximab, and eculizumab.
- Thymectomy Located in the middle upper chest between the lungs, the thymus gland is believed to play a role in the autoimmune response in MG. During a thymectomy, the gland is surgically removed. A randomized controlled trial showed that thymectomy is effective in reducing the dose of prednisone (an immunosuppressive medication) needed by a specific subset of people with MG.
- Methotrexate did not reduce the need for prednisone in a randomized controlled trial of people who have MG with AchR antibodies.
- Rituximab is helpful for people with MuSK MG, according to the consensus report, but less so for those with AchR MG.
- Eculizumab is a new drug with a novel mechanism of action found to improve physical function in people with MG who had not responded to previous treatments. Immunization against meningococcus (a group of bacteria that cause meningitis) is necessary prior to treatment. Eculizumab is given through an injection into a vein once a week for five weeks, then every two weeks after this initial period.
Many people with autoimmune MG need long-term immunosuppressive treatment to help them manage their disorder. The best options for treatment are decided through monitoring the course of the disease and response to treatments over time.
The treatment of MG is complex. Your neurology team will take into account several factors, including age, gender, pregnancy and breastfeeding, and other illnesses (such as high blood pressure, diabetes, or liver disease). They’ll also consider the presence and type of MG antibodies, the type of MG you’re experiencing (ocular MG or generalized MG, which affects more than the eyes alone), and your preferences and values.
As new information about treatment becomes available, discuss possible treatment changes with your neurologist, who can help ensure that the treatment choices you make align with your goals for improvement, as well as your personal values and preferences.
The post How is treatment for myasthenia gravis evolving? appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/how-is-treatment-for-myasthenia-gravis-evolving-2021041222358
via IFTTT
How is treatment for myasthenia gravis evolving?
Friday, 9 April 2021

Easy veggie burgers with a delicious hint of smoky spice. Greek yogurt boosts protein to 10g, but add a fried egg for more!
The post Chipotle Black Bean Burgers With Avocado Salsa appeared first on MyFitnessPal Blog.
from MyFitnessPal Blog https://blog.myfitnesspal.com/watch/chipotle-black-bean-burgers-with-avocado-salsa/
via IFTTT
Chipotle Black Bean Burgers With Avocado Salsa
Often when people think of perimenopause, irregular periods and hot flashes come to mind. But some women may notice another symptom: brain fog.
You’re reading a letter and suddenly realize your thoughts have drifted off and you need to start again. Or you draw a blank when you’re trying to remember someone’s name, or find yourself standing in a room, wondering what you came there to get.
The good news is that these small cognitive blips are probably not anything you need to worry about long-term.
Sleep disturbances and stress may be part of brain fog
Those times when you are less focused and a bit forgetful are likely not just due to hormonal changes. Sleep quality, perhaps related to night sweats during perimenopause, could definitely contribute. Increased stress that sometimes accompanies this stage of life may also have you feeling frazzled and distracted. These factors can interfere with concentration and memory.
Not getting enough sleep can leave you feeling cranky and sluggish. This may be why you can’t remember what’s-her-name: you weren’t paying close enough attention when she told you her name in the first place.
Stress can have a similar effect by pulling your thoughts off task, because you’re preoccupied, worrying about something else.
What can you do to feel less foggy?
If this sounds like you, there are some things you can do to help lift the fog and get your brain re-engaged.
- Slow down. Train yourself to recognize when you’re distracted, and take a moment to breathe and refocus on the task at hand. If you’ve just taken in some new information, try to find a quiet moment to give your brain a chance to process what you’ve learned.
- Manage your stress. Using mindful meditation or other stress-reduction strategies can also help you to relax and be more present. This can help you absorb new information and recall it more easily.
- Get regular exercise. Physical activity benefits not only your body, but also your mind. One study found that just three days a week of moderate-intensity exercise appeared to increase the size of the hippocampus, a part of the brain involved in memory and learning.
- Improve your sleep habits. If you are experiencing poor sleep quality, work on strategies that can help you get more rest at night. Improve your sleep hygiene by making changes, such as staying off electronic devices close to bedtime and establishing a regular sleep schedule. Check with your doctor if at-home strategies aren’t doing the trick.
- Use memory tricks. Did you ever use little tricks to remember things when you were studying for a test in school? Those same mental cheats can help you now as well. For example, make up a mnemonic or a rhyme to help you recall information. Or try using visual or verbal clues. Repeating information or instructions to yourself or someone else is another way to help your brain store information more effectively.
Know when to seek help
Most small memory lapses are nothing to worry about. If changes due to perimenopause — including irregular periods, trouble sleeping due to night sweats, or brain fog — bother you, talk to your doctor about possible solutions.
It’s also important to call your doctor if
- memory changes come on suddenly, or are accompanied by hallucinations, paranoia, or delusions
- memory lapses might put your safety at risk, such as affecting your driving or forgetting food cooking on the stove.
The post Sleep, stress, or hormones? Brain fog during perimenopause appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/sleep-stress-or-hormones-brain-fog-during-perimenopause-2021040922300
via IFTTT
Sleep, stress, or hormones? Brain fog during perimenopause
In a first, scientists grow humanised kidney: Full report
A study published in the scientific journal Cell Stem Cell has depicted growing humanised kidney inside pigs. Pigs are highly attractive tar...