Tuesday, 11 May 2021
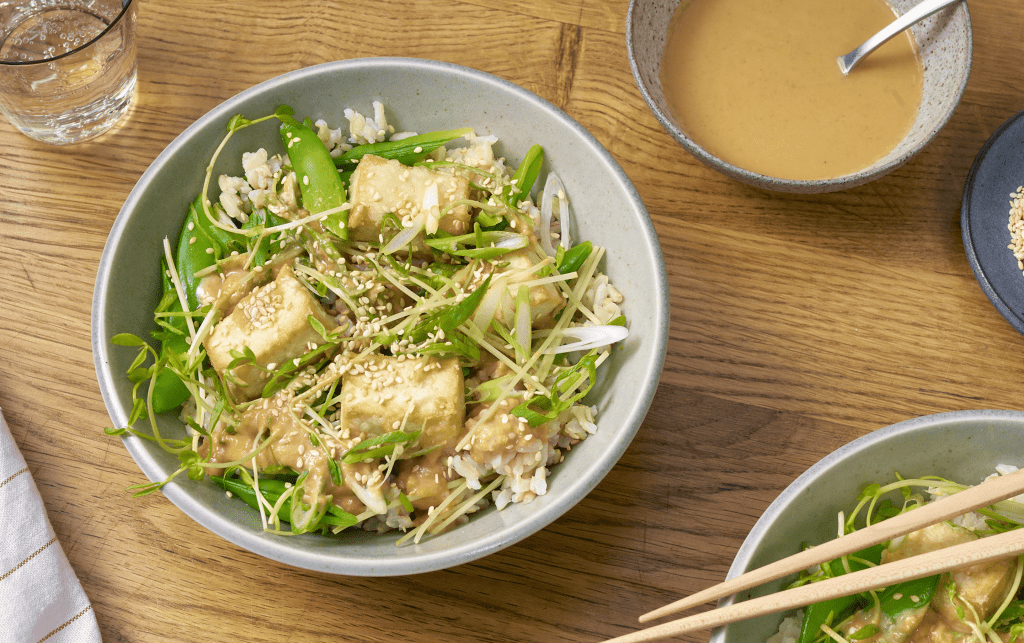
Crispy, oven-baked tofu and snap peas tossed in a sweet & savory sauce of cashew butter, miso paste, soy sauce & honey.
The post Crispy Tofu Bowl With Snap Pea-Miso Salad appeared first on MyFitnessPal Blog.
from MyFitnessPal Blog https://blog.myfitnesspal.com/watch/crispy-tofu-bowl-with-snap-pea-miso-salad/
via IFTTT
Crispy Tofu Bowl With Snap Pea-Miso Salad
Monday, 10 May 2021
Inflammation: if you follow health news, you probably hear about it often. When is inflammation helpful? How can it be harmful? What steps can you take to tone it down?
What is inflammation and how does it affect your body?
If you’re not familiar with the term, inflammation refers to an immune system reaction to an infection or injury. In those instances, inflammation is a beneficial sign that your body is fighting to repair itself by sending in an army of healing white blood cells. As the injury heals or the illness is brought under control, inflammation subsides. You’ve probably seen this happen with a minor ankle sprain: the initial swelling disappears within days as the injury heals.
But inflammation also occurs without serving any healthful purpose, such as when you experience chronic stress, have an autoimmune disorder, or obesity. And instead of solving a problem and receding, inflammation like this can last over a period of time, damaging the body and potentially leading to health problems like arthritis, heart disease, Alzheimer’s disease, depression, and cancer.
This is why inflammation has taken center stage in recent years, and why strategies aimed at reducing it are so popular. Many of these anti-inflammation recommendations relate to your diet.
Can changes in your diet reduce unhelpful inflammation in your body?
The truth is, there are still many unknowns regarding diet and its connection to inflammation and disease. What is clear is that having a healthy diet can help improve overall health and longevity. There is also some evidence to support the notion that eating a host of nutritious foods can reduce inflammation. For example, people who eat lots of fruits and vegetables tend to have lower levels of a substance called C-reactive protein, a marker of inflammation inside the body.
In addition, some research has found a link between diets heavy in foods that promote inflammation and a higher risk of certain health problems. For example, a study in Journal of the American College of Cardiology found that people who consumed pro-inflammatory foods, including red and processed meat, refined carbohydrates, and sugar-laden beverages, were more likely to develop cardiovascular disease than those who regularly reached for anti-inflammatory foods, such as leafy greens, beans, and tea.
It may be too soon to draw a direct line between the food you eat and levels of inflammation in your body. Fortunately, the foods that appear to reduce inflammation also tend to be good for you for other reasons. So, focusing on eating these foods can likely benefit your body in more than one way.
5 food swaps to help fight inflammation
A complete overhaul of your diet is challenging, so experts advise making smaller changes over time. Trying a series of simple swaps may add up to better health in the long term.
Below are five substitutions you can use to help reduce the number of inflammation-promoting foods in your diet.
- Instead of a plain bagel with cream cheese, have a slice or two of whole-grain toast drizzled with olive oil. Whole grains contain substances that help promote the growth of healthy bacteria inside your body. That bacteria may then produce compounds that help to counteract inflammation. Regular consumption of olive oil also has benefits: along with anti-inflammatory effects, it may also help lower blood pressure and improve cholesterol levels.
- Instead of a carbonated soda, try a cup of green tea. Green tea contains substances called catechins, a flavanol thought to combat inflammation. (Just be careful not to load your cup down with sugar.)
- Instead of a corn muffin, substitute a handful of unsalted mixed nuts and an apple. Nuts bring a number of health benefits, including offering up a dose of healthy fats, protein, and (depending on the variety of nuts you are eating) phytochemicals. These phytochemicals contain antioxidants, which help clean up harmful substances called free radicals in the body. They are thought to have anti-inflammatory properties, as well. Fruit such as apples also contains fiber and phytochemicals.
- Instead of a steak and baked potato, have a serving of salmon with a side of broccoli. The omega-3 fatty acids in salmon and other types of fish, such as tuna, sardines, and mackerel, have been linked with better heart health, possibly due to their anti-inflammatory properties. Broccoli is also a good source of fiber and is rich in vitamins C, E, K, and folate. It also contains carotenoids, a phytochemical.
- Instead of a slice of cake, mix up a fruit salad using various types of berries. Fruits such as berries are rich in vitamins and inflammation-busting phytochemicals.
The post 5 inflammation-fighting food swaps appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/5-inflammation-fighting-food-swaps-2021051022570
via IFTTT
5 inflammation-fighting food swaps
Friday, 7 May 2021
As many people know, inflammatory bowel disease (IBD) is a complex condition affecting the intestine, which is the part of the digestive tract that helps digest food and remove water, salt, and waste.
But you might not know this: in recent years in the US, IBD is being diagnosed more often among people who are Black, Hispanic/Latinx, East and Southeast Asian, or from other minority groups than it was in past decades.
Is this a true rise in cases? Is IBD underrecognized in minority populations? While we don’t have all the answers yet, exploring health disparities in IBD and explaining its symptoms may encourage more people to get the health care they need.
What is IBD?
IBD is a chronic inflammatory condition in the intestine that may steadily progress, or repeatedly flare up (relapse) and calm down (remit).
The two main types of IBD are ulcerative colitis (UC) and Crohn’s disease (CD):
- Ulcerative colitis affects the rectum and colon alone.
- Crohn’s disease can affect any portion of the intestinal tract from the mouth to the anus, and can lead to complications such as abscesses, strictures, and fistulas.
- Both conditions frequently involve organs outside of the gastrointestinal tract, such as the joints, skin, and eyes.
What do we know about IBD among minority groups?
Traditionally, IBD has been thought of as a disease that largely affects people who are white. For every 100,000 individuals, IBD occurs in about 10 Hispanic/Latinx individuals, 25 Black individuals, and 70 non-Hispanic white individuals, according to estimates published in 2014. However, more recently we’ve observed an increase in IBD among other racial and ethnic groups in the US and across the world.
Is inflammatory bowel disease underrecognized in minority groups?
Some experts believe that IBD might be underrecognized or underappreciated in minority populations, which might lead to delays in diagnoses. A delayed diagnosis could mean longer periods of untreated inflammation, which also increases risk for complications, such as
- strictures (areas where the bowel narrows due to scarring)
- fistulas (a passage between organs or nearby tissues that isn’t normally there)
- abscesses (an infection that may result in a fistula if not treated)
- surgery
- cancer of the bowel.
One study looked at people receiving health care who had two symptoms suggestive of IBD: iron deficiency anemia (a low red blood count) and diarrhea. The researchers found that certain groups were less likely to receive an appropriate workup to find out why they had these particular symptoms. Those who were Black or publicly insured were less likely to receive the appropriate workup, compared with those who were white or privately insured. These findings further support the hypothesis that IBD might be underrecognized in minority populations.
What do we currently know about health disparities in IBD?
Preventable differences — called health disparities — in health and well-being are seen among people with inflammatory bowel disease. These disparities may be due to a range of factors affecting certain groups, including inequities in the social determinants of health, unconscious biases of medical providers, barriers to care, and differences in the complex genetic and environmental driving forces of IBD that haven’t been sufficiently studied.
Black patients who have IBD experience higher rates of emergency department use — and, in one study, higher rates of hospitalization, possibly because they are less likely to receive regular care from a gastroenterology specialist. Further, while the hospitalization rate in white patients with IBD has decreased, it remains unchanged for Black patients.
Additional research shows that Black patients with Crohn’s disease are less likely to be in remission, more likely to undergo surgery, and more likely to experience complications after surgery. Socioeconomic status matters, too: lower income is linked with a higher risk of severe disease, IBD-related hospitalizations, ICU stays, and death. Another study reports that approximately 14% of Americans with IBD are food insecure. Further, it links food insecurity with inability to take prescribed medications because of cost and difficulty paying medical bills.
What symptoms may be signs of inflammatory bowel disease?
A variety of symptoms may be signs of inflammatory bowel disease:
- Blood in your stool, and urgency and increased frequency of bowel movements, may be signs of ulcerative colitis.
- Abdominal pain, nausea, vomiting, blood in your stool, and diarrhea may be signs of Crohn’s disease.
If you have any of these symptoms — especially if you notice blood in your stool — talk to your healthcare provider. After a medical history and exam, the next steps may be further evaluation with a colonoscopy to look at the bowel, and/or an upper endoscopy to look at the upper part of the digestive system. Imaging studies may also be necessary. This evaluation will help your health provider diagnose IBD or another health problem causing similar symptoms.
Getting effective treatment makes a difference
Fortunately, ulcerative colitis and Crohn’s disease are both treatable conditions. Our goal in treating IBD is stable remission to stop or ease symptoms and ensure a high quality of life. Everyone with IBD can attain this with good care. Treatment may include medicine taken by mouth or given as infusions, dietary changes, surgery, or a combination of these. It’s important to find the right treatment and monitoring plan for each person early in the course of their illness.
I assure my IBD patients that we will work together to find the best and safest treatment options for them. IBD care requires a team approach, which might include a primary care doctor, gastroenterologist, pharmacist, surgeon, dietitian, and other health providers. If you have IBD, you’re the central member and captain of the team; as providers we are just coaches. It is important that you feel heard, understood, and empowered as you navigate life with IBD.
Follow me on Twitter @AdjoaGIMD
The post Is IBD an underrecognized health problem in minority groups? appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/is-ibd-an-underrecognized-health-problem-in-minority-groups-2021050722537
via IFTTT
Is IBD an underrecognized health problem in minority groups?
Thursday, 6 May 2021
If you’ve learned that your newborn or young child has sickle cell disease, you — and other family members and friends — may have many questions.
These days, most cases of sickle cell disease in the US are diagnosed through newborn screening. It’s important to make the diagnosis early, so that babies can be started on penicillin (or another antibiotic) to prevent infection. Getting connected early to a pediatrician for primary care — and to specialists in blood disorders who can work closely with the child as they grow, and with their families — can help prevent complications of the disease.
The basics
Hemoglobin is the part of the red blood cell that carries oxygen. In sickle cell disease, the hemoglobin can change the rounded shape of red blood cells into a C-shape that is crooked, like the tool called a sickle. When that happens, the cells get sticky and can clog up small blood vessels. It also makes the red cells more fragile and likely to break apart, causing anemia.
Millions of people around the world have sickle cell disease, or SCD. In the US, the Centers for Disease Control and Prevention (CDC) estimate it affects about 100,000 people. It occurs in about one out of 365 Black or African American births, and one out of 16,300 Hispanic American births.
Is SCD a genetic disease?
Yes. All of us have two genes that decide what kind of hemoglobin we have, one from each parent. People with sickle cell disease have two copies of the sickle gene, inherited from both parents. If someone has one copy, they have “sickle cell trait,” meaning that they are a carrier of the gene.
Sickle cell trait is common, affecting one in 13 Black children. While there are some problems associated with sickle cell trait, people with sickle cell trait are generally healthy; in fact, they are thought to be less likely to develop severe cases of malaria, which is why the disease was thought to have evolved in people from areas around the equator where malaria is common.
There are other kinds of genetic hemoglobin diseases, such as thalassemia or hemoglobin C. Sometimes people are born with one sickle gene and one gene for a different hemoglobin problem. The severity of their condition depends on the particular hemoglobin combination.
Currently, there is no cure for sickle cell disease or the other genetic hemoglobin diseases, except for bone marrow transplant or stem cell transplant.
What health issues could SCD cause?
When sickle cells clog up blood vessels, it can lead to pain and damage to organs or tissues due to lack of blood flow. When coupled with the effects of anemia, this means that babies and children with sickle cell disease are more likely to have complications from infections, such as pneumonia; vision problems; blood clots; and breathing problems. Children with sickle cell disease can also get swelling of the spleen if sickled cells get stuck there.
How can you help your child live a healthy life as they grow?
Children with sickle cell disease and their families can work together to help prevent complications by taking these steps:
- Stay well-hydrated, as dehydration can make cells more likely to sickle.
- Avoid extremes of temperature, especially cold, as this also can trigger sickling of the cells.
- Avoid areas of high altitude, where there is less oxygen.
- Take care with very vigorous exercise, which may decrease the amount of oxygen available to the blood.
- Wash hands regularly and avoid sick people to the extent possible.
- Get all recommended vaccinations.
- Learn all the signs and symptoms of blocked blood vessels, anemia, a swollen spleen, infection, blood clots, and lung problems, so that they know when to get medical care immediately. Ask your child’s doctor or medical team to help you understand key warning signs for each of these based on your child’s age.
Also, see this helpful toolkit created by the CDC and the American Society of Hematology. It explains common complications of sickle cell disease and steps to take for better health.
Being closely connected to medical care is crucial, because the sooner complications are diagnosed, the sooner and more successfully they are treated. There are also treatments such as hydroxyurea that can help prevent complications in the first place. Children with sickle cell disease should regularly see their primary care pediatrician and their specialist, whether they are having symptoms or not, so that they can work together to help live the healthiest life possible.
Follow me on Twitter @drClaire
The post Sickle cell disease in newborns and children: What families should know and do appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/sickle-cell-disease-in-newborns-and-children-what-families-should-know-and-do-2021050622545
via IFTTT
Sickle cell disease in newborns and children: What families should know and do
Wednesday, 5 May 2021
Vaccines have been heralded as a key measure to slow the COVID-19 pandemic and one day bring it to an end. Every day, millions of American adults are receiving one of the authorized vaccines proven highly effective at preventing severe illness that might otherwise lead to hospitalizations and deaths. In the US, most people over 65 have now been fully vaccinated, protecting the most vulnerable in our population.
As an infectious disease specialist, my responses to the questions below are based on what we know so far about infection and vaccines in children and teens. We’ll need to continue filling in gaps as research is done and our understanding evolves.
What do we know about how COVID-19 affects children and teens?
Most COVID-19 infections in children are mild or cause no obvious symptoms. However, a small percentage of infected children
- develop a serious inflammatory condition called MIS-C in the two to six weeks following COVID-19 infection. This may happen even in children who have mild symptoms or no symptoms.
- get very sick and need hospitalization or intensive care.
Over 400 children have died from COVID-19 infection. That’s greater than the number of childhood deaths during the deadliest flu season in the past two decades.
Vaccinating children to prevent these outcomes is one of the most important reasons driving vaccine studies in children. Further, vaccinating children will be critical to achieving a population-wide level of immunity — herd immunity — sufficient to slow the emergence of dangerous variants and bring an end to the pandemic.
What do we know so far about COVID-19 vaccines in teens?
- The Pfizer/BioNTech vaccine is authorized for use in people ages 16 and older.
- The Moderna and Johnson & Johnson vaccines are authorized for use in people ages 18 and older.
- These authorizations were based on data from participants of these ages in randomized, placebo-controlled trials that demonstrated the safety and efficacy of these vaccines. Efficacy measures how well a vaccine works in the controlled circumstances of a study. Effectiveness is how well a vaccine works outside of a study, when people in the community receive it.
As states expand eligibility for COVID-19 vaccines, teens 16 and older can receive the appropriate vaccine through the same sources adults have had access to so far. Available vaccine sites may vary by state and where you receive health care. Check the searchable map on VaccineFinder, or your state board of health.
Vaccine research done so far, or now underway, includes the following:
- Pfizer/BioNTech has completed a trial in 12-to 15-year-olds. This trial used the same dose and schedule of the vaccine as is used in adults: two doses given three weeks apart. The company announced in a press release that the vaccine was safe and well tolerated, elicited strong antibody responses, and had 100% efficacy in preventing mild to severe infection in this age group. The FDA is reviewing the data and will consider authorizing this vaccine for use in this age group. If all goes well, we might expect this vaccine to be available to 12-to 15-year-olds in the coming months.
- Moderna completed enrolling 12-to 17-year-olds in a similar trial using the same dose and schedule as in adults: two doses given four weeks apart. Data from this trial are expected within the next few months.
- Johnson & Johnson has started a trial of its vaccine for a small number of 16-to 17-year-olds. If the vaccine proves to be safe and effective in that age group, the trial will continue with 12-to 15-year-olds.
What about COVID-19 vaccine trials for younger children?
- Pfizer/BioNTech and Moderna have both begun trials in children 6 months to 11 years old.
- These trials will each begin by testing smaller doses than those given to older children, teens, and adults. This allows researchers to determine which dose is well tolerated and still elicits strong antibody results in younger children.
- Once the dose is set, larger numbers of children in these age ranges will be enrolled in placebo-controlled trials to evaluate the efficacy of these vaccines.
All of these steps will take some time so that they can be done without cutting any corners on safety. The earliest vaccines will likely be available for younger children is late 2021, or perhaps early in 2022.
What is not yet known about COVID-19 vaccines in children and teens?
- How long vaccine-induced immunity against COVID-19 infection lasts in children will need to be followed over time. Findings from such studies will help experts decide whether children will need boosters of COVID-19 vaccines in the future.
- Researchers also need to study whether COVID-19 vaccines can be combined with other vaccines that children routinely receive. For now, the CDC recommends not giving any other vaccines within 14 days of a COVID-19 vaccine. This is true for people of any age.
- Researchers will need to evaluate the impact of these vaccines on protecting children from infection with COVID-19 variants. But biologically, there would be no reason to expect differences in vaccine coverage of variants in adults versus children.
The post COVID-19 vaccines for children and teens: What we do — and don’t — know appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/covid-19-vaccines-for-children-and-teens-what-we-do-and-dont-know-2021050522523
via IFTTT
COVID-19 vaccines for children and teens: What we do — and don’t — know
Tuesday, 4 May 2021
While the COVID-19 pandemic is not over by any means, more people are getting vaccinated, and restrictions are gradually lifting. After too much time spent inactive and indoors, what better way to move your body and enjoy nature than by taking a hike? In many ways, hiking is the ideal antidote to a global pandemic, as it can heal both body and soul.
Enjoy the benefits of a hike
- Like power walking, hiking offers a moderate-intensity cardio workout, provided your route includes some hills or inclines. Trekking on uneven surfaces engages your core muscles and improves your balance.
- Hiking also is a mood booster. Research shows that spending time in green spaces, like nature trails and wooded areas, can reduce stress, anxiety, and depression. It doesn’t matter if you hike alone or with others.
- The CDC still suggests people maintain social distancing during outdoor activities, including hiking, since it’s not possible to know who is fully vaccinated. You also should wear a mask around people who are not in your household or in your personal pod.
- Many local, state, and national parks are still closed or have limited access, but some trails may be open in your area or will reopen soon. (Check out these sites to find the status of local trails near you: National Park Service, American Trails, and American Hiking Society.)
Ready to hike?
Before you lace up your hiking boots, make sure you’re well prepared. After all, it’s probably been a while since you’ve been out in the world. Here are some tips.
Work on your walking. If your walking endurance needs some work, begin a regular walking program in your neighborhood. Walk daily for 10 to 20 minutes, and wear a step counter to motivate you.
Safety first. If you can’t hike with someone, let a friend or family member know where you will hike and for how long. Bring your cell phone and a local map, if needed.
Apply sunscreen. Even if you mostly hike in the shade, you can still get sunburned. Always wear sunscreen with at least 30 SPF that blocks both types of ultraviolet rays — UVA and UVB —and a lip balm with sunscreen. Apply about 20 minutes before your hike, and then reapply every two hours.
Protect against ticks. Ticks are common in the US and can spread serious illnesses, such as Lyme disease and Rocky Mountain spotted fever. Ticks are often found in wooded, bushy, or grassy areas. Wear light-colored clothes with long sleeves and long pants, if possible. Use insect repellent that is effective against ticks on exposed skin, clothes, and hiking gear. Do a thorough tick check after hiking. Know what to do if you find a tick on your body — and what signs suggest you might have been bitten by one, such as a rash or flulike symptoms. Contact your health provider right away for advice and appropriate treatment.
Stay hydrated. Drink water before, during, and after your hike. Pay attention to your thirst (if you are thirsty, you are likely already dehydrated.) Set a timer on your phone or sports watch to remind you to drink at regular intervals.
Watch the weather. If you are not sure about the forecast, wear layers that you can add or take off depending on the temperature. Carry a rolled-up windbreaker, rain jacket, or poncho in a backpack.
Support yourself. Invest in hiking or trail shoes with good ankle support. Wear calf-length socks to protect your legs. Hiking with walking poles can help you navigate tricky terrain and support your knees.
The post Happy trails: Take a hike, now appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/happy-trails-take-a-hike-now-2021050422511
via IFTTT
Happy trails: Take a hike, now
In a recent blog post I discussed how beneficial sleep is for memory function. But sleep isn’t just good for your memory; it can actually reduce your risk of dementia — and death. Although it has been known for some time that individuals with dementia frequently have poor, fragmented sleep, two new studies suggest that if you don’t get enough sleep, you are at increased risk for dementia.
Sleep six to eight hours each night
In the first study, researchers at Harvard Medical School studied more than 2,800 individuals ages 65 and older participating in the National Health and Aging Trends Study to examine the relationship between their self-report of sleep characteristics in 2013 or 2014, and their development of dementia and/or death five years later. Researchers found that individuals who slept fewer than five hours per night were twice as likely to develop dementia, and twice as likely to die, compared to those who slept six to eight hours per night. This study controlled for demographic characteristics including age, marital status, race, education, health conditions, and body weight.
In the second study, researchers in Europe (including France, the United Kingdom, the Netherlands, and Finland) examined data from almost 8,000 participants from a different study and found that consistently sleeping six hours or less at age 50, 60, and 70 was associated with a 30% increase in dementia risk compared to a normal sleep duration of seven hours. The mean age of dementia diagnosis was 77 years. This study controlled for sociodemographic, behavioral, cardiometabolic, and mental health factors, although most participants were white, better educated, and healthier than the general population. In addition, approximately half of the participants had their sleep duration measured objectively using a wearable accelerometer — a device that tracked their sleep using body movements — which confirmed the questionnaire data.
Inadequate sleep in midlife may lead to dementia
What’s new here is that inadequate sleep in midlife raises one’s risk of dementia. There are many reasons for poor sleep in middle age: shift work, insomnia, caretaking responsibilities, anxiety, and pressing deadlines, just to name a few. Although not all of these are controllable, some are. For example, if you’re currently only sleeping four to five hours because you’re up late working every night, you might want to change your habits, otherwise you risk developing dementia by the time you retire!
This relationship between sleep in midlife and dementia in late life is important not only from a clinical perspective, but also from a scientific one. It had always been a bit of a chicken-and-egg problem when trying to interpret the relationship between poor sleep and dementia. Was it really poor sleep that caused dementia, or just early dementia symptoms causing poor sleep? By looking at individuals who were initially studied in midlife — some as young as age 50 — we now have greater certainty that poor sleep can increase one’s risk of developing dementia 25 years or more in the future.
Flush your brain while you sleep
Although it is not totally understood why inadequate sleep increases your dementia risk, one possible reason relates to the deposition of the Alzheimer’s protein, beta amyloid. Beta amyloid is the protein that clusters and clumps together to form Alzheimer’s plaques. No one is completely certain what its normal function is, although there is increasing evidence it is involved in the brain’s defense against invading microorganisms.
During the day, we all make some of this beta amyloid protein in the brain. When we sleep, however, brain cells and their connections actually shrink. This shrinking allows more space between the brain cells, so that beta amyloid and other substances that accumulate during the day can be flushed away.
So the theory is, if you don’t get enough sleep, your brain won’t have enough time to drain away beta amyloid and other substances. These substances then continue to accumulate, day after day, until they cause dementia.
The good news
The good news is that you can reduce your risk of developing dementia by getting adequate sleep. One study from researchers in Toronto and Chicago examined people who were at increased genetic risk of developing Alzheimer’s. They found that better sleep not only reduced the likelihood of developing clinical Alzheimer’s disease, but it also reduced the development of tangle pathology in the brain — another substance that accumulates in Alzheimer’s disease.
The bottom line
Sleep isn’t merely an annoying interruption between the important aspects of our waking lives. Just like eating right and exercising, sleep is absolutely essential for good brain health. These two new studies show that the harmful effects of inadequate sleep can start at age 50 (if not earlier), and they can lead to early dementia and death. But the good news is that you can reduce your risk of dementia by simply giving yourself six to eight hours of sleep each night. Try to avoid sleeping pills, as they don’t give you the deep sleep you need. If you’re having trouble sleeping, nonpharmacological approaches are best.
The post Sleep well — and reduce your risk of dementia and death appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/sleep-well-and-reduce-your-risk-of-dementia-and-death-2021050322508
via IFTTT
Sleep well — and reduce your risk of dementia and death

Zesty Mexican-inspired soup with an easy base of jarred green salsa, plus canned chickpeas for extra protein and fiber.
The post Chickpea Posole Verde appeared first on MyFitnessPal Blog.
from MyFitnessPal Blog https://blog.myfitnesspal.com/watch/chickpea-posole-verde/
via IFTTT
Chickpea Posole Verde
Saturday, 1 May 2021
I have a confession: in late 2020, when the first COVID-19 vaccines were approved by the FDA, I was hesitant to get one myself. Despite working in public health and believing strongly in vaccines to keep our community healthy, I was anxious about putting something in my body that seemed so new. I thought: “What if the vaccine is dangerous?” “What about long-term side effects?”
I am part of the LGBTQ+ community. Our history may help explain why I hesitated.
Are LGBTQ+ people more hesitant to get the vaccine?
In March a New York Times article reported that LGBTQ+ people are more hesitant to get the COVID-19 vaccine. A research study from the Human Rights Campaign reported mixed findings: while LGBTQ+ people overall are more likely to get vaccinated, certain subgroups, such as LGBTQ+ people of color and bisexual women, are less likely to get vaccinated.
LGBTQ+ people have good reason to be hesitant about vaccines. Historically, this population has experienced — and continues to experience — discrimination in multiple settings, including in healthcare. At the same time, this population is more vulnerable to COVID-19 (see this study and an earlier blog post I wrote). LGBTQ+ people who are also people of color may be even more hesitant to get the COVID-19 vaccine, because of trauma and oppressions based on multiple intersecting marginalized identities that set the stage for mistrust in healthcare and medical research. We can include racism, transphobia, biphobia, and homophobia among such oppressions.
Weighing the risks and benefits of the COVID-19 vaccine
When I was trying to decide whether to get the vaccine, I began reading about the vaccine from trusted sources like the Centers for Disease Control and Prevention (CDC). I also talked to people I know and trust, like close friends, family members, and physician colleagues. I asked them: “Will you get the vaccine when it’s offered to you?” All of them gave me a resounding “yes!” Most shared this rationale: while we still don’t know about long-term side effects, this vaccine is similar to other vaccines that have been around for a while, and the benefits of getting vaccinated far outweigh the risks of getting seriously ill or even dying from COVID-19.
When the vaccine was offered to me earlier this year, I booked my appointment immediately, without hesitation, and I haven’t looked back. As soon as I got the first shot, and certainly when I was fully vaccinated two weeks after my second shot, I felt a profound sense of relief. I also felt empowered about taking an important step toward keeping myself, my family, and my community safe from COVID-19. I now feel safer and freer in my daily life. I go into stores (wearing a mask) without feeling anxious, and I have been able to visit in-person with other fully vaccinated people, like my mom, without masks.
If you are struggling to decide whether to get the COVID-19 vaccine, this decision-making grid may be helpful (note: auto-download). The grid walks you through the benefits and short-term and long-term risks of not getting the vaccine compared to getting the currently available vaccines.
Why the vaccine is critical for LGBTQ+ communities
Numerous “pandemics” have already wiped out large numbers of the LGBTQ+ community: HIV/AIDS, violence, suicide. In addition, the COVID-19 pandemic has already disproportionately harmed LGBTQ+ people (see this study and this report). LGBTQ+ seniors and people of color are at greatest risk for serious, possibly life-threatening illness from COVID-19. If each of us takes steps to get vaccinated, we can prevent more deaths and negative health outcomes in our communities.
How can you empower yourself to get the COVID-19 vaccine?
- Educate yourself on what COVID-19 vaccines are, how they work, and why they are safe.
- Talk to trusted experts and people in your life about your fears.
- At this time, everyone in the US who is age 16 or older is eligible for the vaccine, so you can make an appointment where you live to get vaccinated.
Additional resources
- More info on COVID-19 and vaccines:
- Ways to avoid COVID-19 vaccine scams
- What you can do after you are vaccinated
The post COVID-19 vaccines and the LGBTQ+ community appeared first on Harvard Health Blog.
from Harvard Health Blog https://www.health.harvard.edu/blog/covid-19-vaccines-and-the-lgbtq-community-2021043022482
via IFTTT
COVID-19 vaccines and the LGBTQ+ community
In a first, scientists grow humanised kidney: Full report
A study published in the scientific journal Cell Stem Cell has depicted growing humanised kidney inside pigs. Pigs are highly attractive tar...